
Every year, Medicare Advantage organizations (MAOs) undergo a grueling process to prepare for the Annual Enrollment Period (AEP). For Medicare, the AEP runs from October 15th to December 7th. During the AEP, beneficiaries may add, change, or drop their Medicare Part D or Medicare Advantage plan coverage for the coming year. Before it begins, MAOs must update their plan materials according to strict CMS guidelines and timelines.
The Center for Medicare and Medicaid Services (CMS) requires that before the AEP begins, every MAO must have specific Medicare communications ready for and available to both existing and potential Medicare beneficiaries, through print and digital channels and multiple languages. The CMS also sets out stringent requirements for the plans, content, and layouts, and each year MAOs must make adjustments and changes to their own plans as required.
CMS-regulated documents are very complex. In particular, The Annual Notice of Change (ANOC), Evidence of Coverage (EOC), and Summary of Benefit (SB) are elaborate and complicated. Every spring, the CMS hands down new language and models which MAOs then use to amend their own plans.
It’s an intricate procedure. MAOs face several ongoing obstacles when it comes to the preparation of regulated materials. First, tight deadlines. MAOs must amend all of their plans, some of which might cover thousands of beneficiaries across multiple states, within the time given. That restricted time frame can lead to the second hurdle, the potential for errors, the effects of which are compounded by fines and the rework necessary to correct errata. Finally, the complexity of the documents is in itself a challenge. CMS specifications are exacting and precise, and an absolute requirement.
MAOs can choose from several different tactics to manage the annual update of these complex, regulated materials. Manual approaches, whether created in-house by desktop tools or outsourced to a third party, are inefficient and introduce risk to the process. Any human error, cut-and-paste inaccuracy, or lapse in version control can cause significant complications and lead to costly delays and damages. Regardless of the approach, none of these provide economies of scale, so as the number of plans under management grows, so do the headaches.
Error-ridden or non-compliant material can result not only in the potential for missed CMS deadlines with all the fines that entails, but also can result in expensive reprints and remailings. In addition, there are other, less obvious costs of fixing errata. Such as the surge in extra wages and overtime fees to cope with the extra work, and the likely possibility of employee burnout and turnover.
Automation can reduce the time and effort required during the update cycle, without sacrificing accuracy. But IT-driven automated solutions can be cumbersome. When every update requires programmer intervention, delays mount and the possibility of miscommunication introduces new risks.
There’s a better way to handle the pressures of Medicare Advantage plan materials. The Messagepoint Healthcare Touchpoint Exchange streamlines the entire cycle from end to end, and helps you ensure compliance while giving you more visibility and control. Simplify your process with automation accessible to business users that assures your accuracy and reduces your risk, while also enabling you to scale your plans.
Want to learn more? Messagepoint has created videos outlining the 9 best practices for Medicare Advantage plan management relating to:
TORONTO, December 5, 2024 – Messagepoint Inc. announced it has been named a Leader in the IDC MarketScape:…
Read more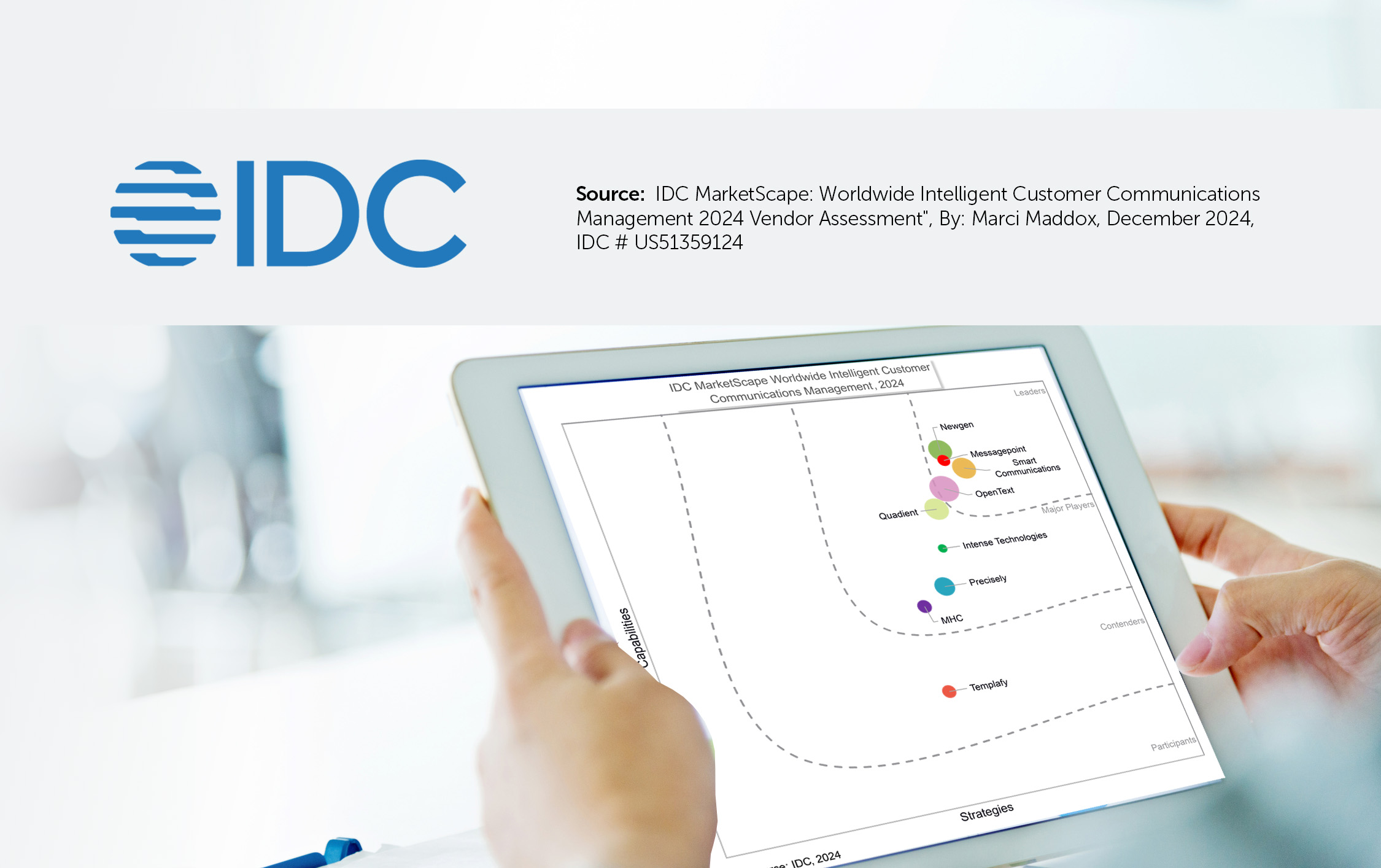
IDC’s MarketScape for Intelligent Customer Communications Management evaluates vendors that natively own or integrate forms technology and artificial…
Read the whitepaper
The mortgage servicing industry is under immense financial pressure. With interest rates high and home prices still rising,…
Read the Article