
With CMS planning to allow an expanding array of covered benefits and the market for Medicare Advantage plans projected to grow from 25 million to 34 million enrolments in five to six years, healthcare payers are seeing unprecedented opportunities to reach new members and positively impact their health and well-being.
We’ve watched the health plan landscape change significantly over the years, evolving from traditional health maintenance organization (HMO) plans to preferred provider organization (PPO) plans to today’s more consumer-driven high-deductible and health savings account (H.S.A.) models. Perhaps in recognition of the increasingly important role of consumers in the current health care marketplace, even the traditionally print-centric Centers for Medicare and Medicaid Services (CMS) is now recognizing the need for communications with health plan members to extend beyond print and into digital channels, including internet portals, email, text, etc.
And with good reason—in the past ten years the number of Medicare members with internet access has risen from 20 percent to more than 70 percent. At the same time, providers have recognized that rather than trying to incentivize behavior, a more successful approach is to build trust through a close partnership with their members.
Building trust and getting members to understand and take advantage of plan benefits is now the key to success for Medicare Advantage payers, but it won’t happen with traditional plan documents, which in many ways are archaic in format and confusing to members. What is needed is a way to parse benefit information into bite-sized, digestible pieces that meaningfully communicate relevant benefits to members. The goal should be to find a way to get a tailored message, driven by real-time data about the member, in the right channel and at the right time.
For example, before a member is seen by a doctor, the medical practice will complete benefit verification for the health plan while scheduling the visit. This eligibility data will indicate what type of provider that a member is going to see, maybe a kidney specialist. In this case, a message could be sent to the member’s smartphone informing them about their dialysis benefits which they may not otherwise have known about. Communications like these that educate members about their benefits will have a positive impact on member experience and reduce grievances that can result in membership churn and reduced Star Ratings. Payers already have real-time clinical data on their members that could drive highly personalized and relevant benefit communications.
However, payers will also need a content management solution that can easily create and deliver those highly variable, and highly complex, benefit level communications. A logical choice to look for these capabilities is with an automated solution that can produce the required annual Annual Notice of Change (ANOC) and Evidence of Coverage (EOC) documents reliably. These documents provide a great foundation for an automated platform, to show it can handle complex documents, and the natural next step would be to extend its capabilities to easily produce other data-driven customer communications like the one described above. The key to doing so in a timely manner will depend on whether the solution can enable business users to create and send rule-based, relevant messages via the channel of the member’s choice without the need to involve IT resources or a downstream print agency that could slow the process. Increasingly these platforms are cloud-based SaaS solutions.
Health plan marketing departments typically create customer acquisition campaigns for a new year and design hundreds of versions of a document with different messaging based on different benefit scenarios. If a plan discovers down the road that one campaign is significantly more successful than another, it may want to adjust its messaging for the less successful campaign. However, if the plan is working with a print vendor that controls the software on which the campaign was designed, it can be difficult and time-consuming to implement the changes. If, on the other hand, the plan’s marketing department can make the changes it desires on its own and easily implement them into new communications, then they will have the agility to be responsive to market conditions.
Similarly, we know of one health plan that has incorporated a way for call center representatives to easily personalize its touchpoints with customers. Once a representative ends a phone session, an automated system generates a letter to the member that the representative can personalize and immediately send. Finding ways to both automate and keep communications with members personal is a goal many health plans share.
Finding solutions of this kind that will promote better member education and experience while at the same time streamlining processes and reducing costs is a strategy that can help Medicare Advantage plans succeed in a promising—but competitive—marketplace.
TORONTO, December 5, 2024 – Messagepoint Inc. announced it has been named a Leader in the IDC MarketScape:…
Read more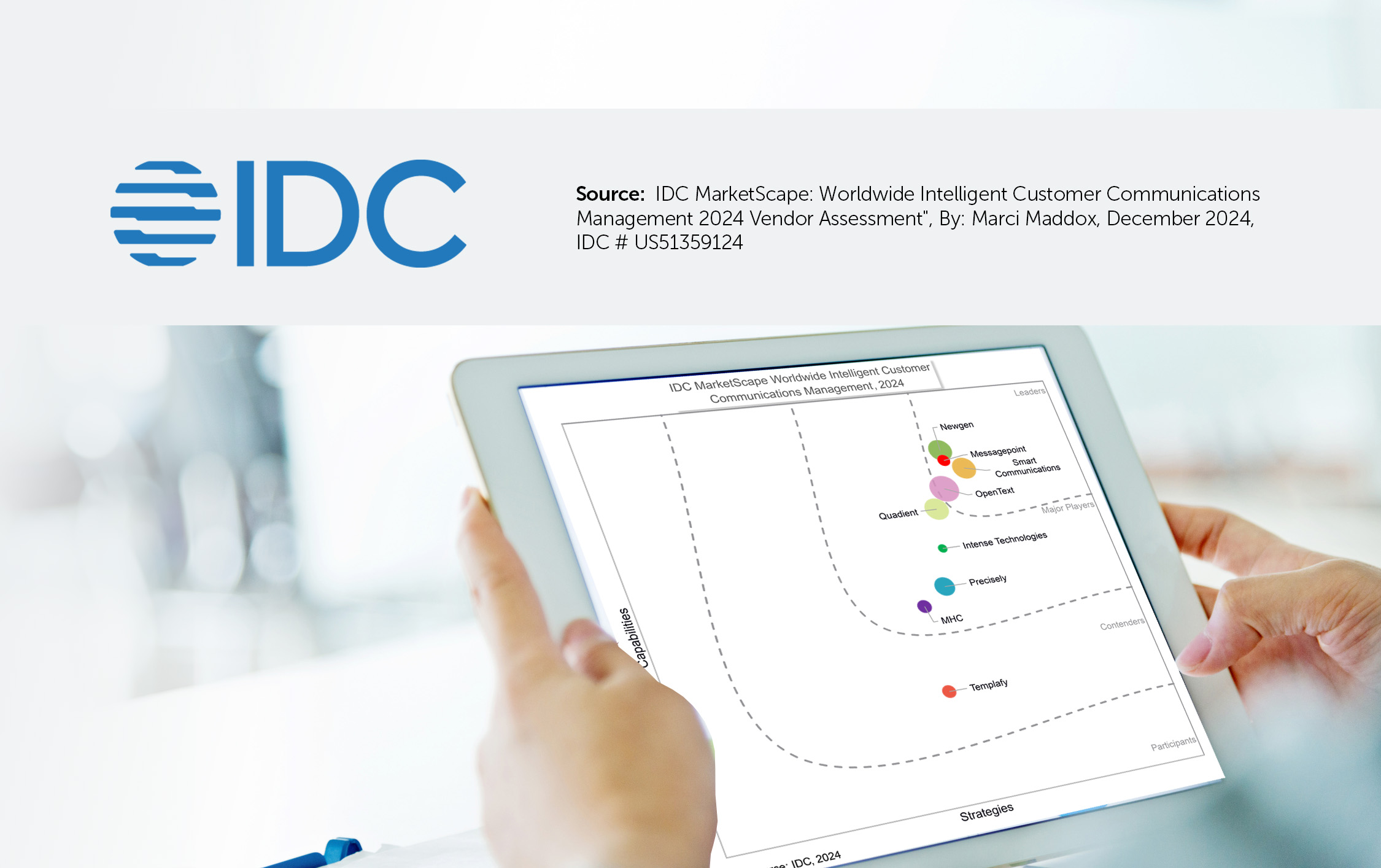
IDC’s MarketScape for Intelligent Customer Communications Management evaluates vendors that natively own or integrate forms technology and artificial…
Read the whitepaper
The mortgage servicing industry is under immense financial pressure. With interest rates high and home prices still rising,…
Read the Article